Heartburn and a feeling of discomfort in the throat are among the main signs of inflammatory processes on the mucous membrane of the esophagus, and need treatment by qualified specialists. Moreover, The symptoms and treatment of esophagitis reflux should always be monitored by doctors. This is the only way to avoid irreversible changes in the tissues of the esophagus, and the development of complications requiring surgical intervention.
Material Content:
Reflux esophagitis: what is it?
Let's try to understand what is esophagitis reflux. “Esophagitis” is an ancient Greek word meaning esophagus. The term "reflux" is borrowed from Latin and is translated as "backward flow."

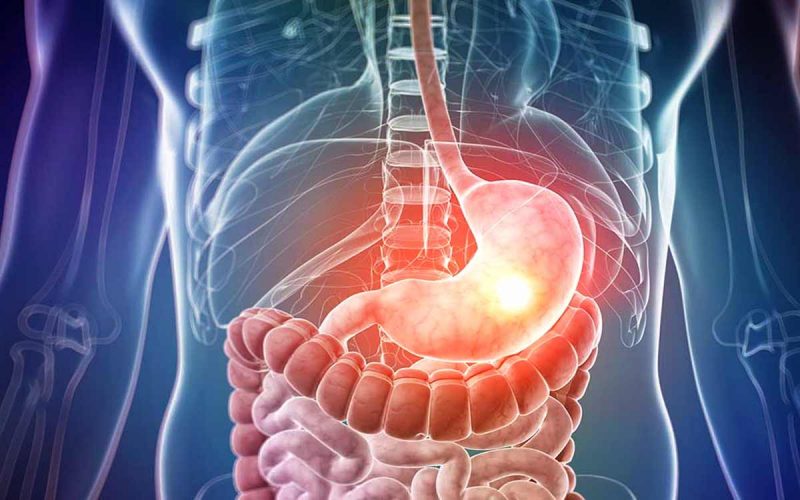
Thus, both concepts reflect the process that occurs during the development of the disease - food masses, gastric juice and enzymes move back from the stomach or intestines, penetrate the esophagus, irritating the mucosa and causing its inflammation.
At the same time, the lower esophageal sphincter, which separates the esophagus and stomach, does not provide the necessary obstacles to the movement of acid masses.
In official medicine, reflux esophagitis is a complication of gastroesophageal reflux disease, which is characterized by the reflux of the acid contents of the stomach or intestines into the esophagus.
A periodically repeated aggressive effect gradually destroys the mucous membrane and epithelium of the esophagus, contributing to the formation of erosive foci and ulcers - potentially dangerous pathological formations that threaten degeneration into malignant tumors.
Causes of occurrence
Under certain circumstances, gastroesophageal reflux can occur in healthy people. Frequent cases of the onset of the disease indicate the development of inflammatory processes in the gastroduodenal region.

Among the possible causes of reflux, gastroenterologists distinguish the following pathological changes in the structure and functionality of the digestive tract:
- decreased tonus and barrier potential of the lower esophagus sphincter;
- violation of esophageal cleansing, redistribution and removal of biological fluids from the intestine;
- violation of the acid-forming mechanism of the stomach;
- decreased mucosal resistance;
- narrowing of the lumen of the esophagus (stenosis);
- an increase in the size of the esophageal opening of the diaphragm (hernia);
- violation of gastric emptying;
- high level of intra-abdominal pressure.
Most often, esophagitis reflux occurs as a result of a weakening of the musculature of the esophagus against the background of an overflowing stomach.
Provocative factors
There are several etiological varieties of factors that provoke the throwing of acid masses into the esophagus: physiological characteristics of the body, pathological conditions, lifestyle.
The development of reflux contribute to:
- pregnancy;
- allergy to certain types of products;
- overeating;
- obesity;
- smoking and alcohol;
- poisoning;
- unbalanced diet;
- stress
- work associated with frequent torso;
- autoimmune diseases;
- taking medications that weaken the muscles of the cardiac sphincter.
In addition, reflux disease can occur as a result of prolonged use of a nosogastric tube.
In men, gastroesophageal reflux is more common than in women, although science has not established a direct relationship between the disease and the gender of the person.
Symptoms and signs of the disease
When gastric masses reach the surface of the mucosa, a burning sensation arises in the esophagus, since exposure to acid causes tissue burns.

With a long course of the disease, the symptoms of esophagitis reflux become more pronounced, and other pathological manifestations are added to heartburn:
- belching sour. It may indicate the development of esophageal stenosis on the background of erosive and ulcerative lesions of the mucosa. The appearance of belching at night is fraught with the ingress of acid masses into the respiratory tract;
- pain in the sternum, often extending to the neck and the area between the shoulder blades. Usually occurs when leaning forward. By clinical characteristics, it resembles the symptoms of angina pectoris;
- difficulties with swallowing solid foods. In most cases, the problem occurs against the background of narrowing of the lumen of the esophagus (stenosis), which is considered as a complication of the disease;
- bleeding - a sign of the extreme degree of development of the disease, requiring urgent surgical intervention;
- foam in the mouth is the result of increased productivity of the salivary glands. It is rarely observed.
In addition to standard clinical signs, extra-esophageal symptoms may indicate the development of the disease.
Signs of extra-esophageal nature
The occurrence of pathological processes in parts of the body that are not directly related to the digestive tract is not always associated with pathological processes in the esophagus - especially against the background of a lack of severe heartburn.
In the absence of full-fledged diagnostic studies, adequate treatment of esophagitis reflux is not possible.
Extra-esophageal symptoms of inflammatory processes on the mucous membrane of the esophagus differ not only in the nature of severity, but also in localization:
- ENT organs. In the early stages of the disease, rhinitis, laryngitis and pharyngitis develop, a feeling of a lump or cramping in the throat appears. As the pathology develops, ulcers, granulomas and polyps can develop in the area of the vocal cords, as a result of which the patient’s voice changes, becomes hoarseness and rudeness. In the later stages of the disease, cancer of the ENT organs is possible;
- oral cavity. On the tissues of the oral cavity, when gastric juice enters, erosive lesions appear, periodontitis, caries and salivation develop. Pathological processes are accompanied by halitosis;
- bronchi. Night attacks of suffocation or severe coughing are possible;
- sternum, heart. Pain in the sternum is identical to the manifestations of coronary heart disease. Perhaps the appearance of additional signs indicating cardiac pathology - hypertension, tachycardia. It is almost impossible to establish the cause of the disease without special diagnostic tests;
- back. Back pain is caused by innervation with the digestive tract, the source of which is located in the sternum of the spine.
In addition, the appearance of symptoms indicating a violation of the functionality of the stomach is possible - nausea, vomiting, bloating, rapid feeling of fullness.
Degrees of Reflux Esophagitis
The level of complexity of the course of the disease is determined by the stages of its development. In most cases, the development of gastroesophageal reflux disease takes about three years, during which the pathology takes one of four forms classified by WHO.
Reflux esophagitis of the 1st degree is characterized by intense redness of the epithelium of the esophagus and the relatively small, up to 5 mm, area of the mucosal lesion area by point erosion.
The second degree of the disease is diagnosed in the presence of erosion and ulcerative sites against the background of edema, thickening and bruising of the mucosa. With vomiting, partial rejection of minor mucosal fragments is possible. The total area of lesions occupies about 40% of the surface of the esophagus.
For the third degree of esophagitis reflux, an increase in the area of damage to 75% of the surface of the esophagus is characteristic. At the same time, ulcerative formations gradually merge into a single whole.
The development of the fourth degree of the disease is accompanied by an increase in the size of the ulcerous areas. Pathological formations occupy more than 75% of the surface of the mucosa and affect the esophageal folds.
If untreated, necrotic processes develop in the tissues of the esophagus, leading to the degeneration of cells into malignant.
Types of disease
The development of esophagitis reflux can occur in acute or chronic form
The acute form of reflux is the result of a burn of the mucosa under the influence of gastric juice. Most often observed in the lower esophagus and responds well to treatment.
The chronic form can occur both against the background of an untreated exacerbation, and in the form of an independent primary process. The chronic course of the disease is characterized by periodic exacerbations and remissions.
Diagnostic measures
Despite the possible severity of the clinical manifestations of esophagitis reflux, additional information is needed to obtain an accurate diagnosis, which is obtained through examination.

The most informative are such studies as:
- blood analysis;
- Analysis of urine;
- radiography of the sternum;
- endoscopy - a procedure that allows to identify erosive and ulcerative formations, as well as other pathological changes in the state of the esophagus;
- biopsy;
- manometric analysis of the state of sphincters;
- scintigraphy - a method for evaluating esophageal self-cleaning;
- pH-meter and impedance pH-meter of the esophagus - methods to assess the level of normal and retrograde motility of the esophagus;
- daily monitoring of the level of acidity in the lower esophagus.
Reflux esophagitis is diagnosed in the presence of histological and morphological changes in the mucous membrane of the esophagus.
Treatment for reflux esophagitis
Successful treatment of esophagitis reflux involves an integrated approach - the use of drug therapy against the background of a change in the patient's lifestyle.
Drug treatment
Prescribing medications for gastroesophageal reflux disease has several tasks - improving the self-cleaning of the esophagus, eliminating the aggressive effects of the gastric masses, and protecting the mucosa.
The following drugs are most effective for treating reflux:
- antacids - Phosphalugel, Gaviscon, Maalox;
- antisecretory drugs - Omeprazole, Esomeprazole, Rabeprazole;
- Prokinetics - Domperidone, Motilium, Metoclopramide.
In addition, vitamin preparations are indicated - pantothenic acid, which stimulates peristalsis and promotes the restoration of the mucosa, as well as methyl methionine sulfonium chloride, which reduces the production of gastric secretion.
Surgical intervention
With the development of reflux of esophagitis of the third and fourth degree, surgical methods of treatment are indicated - an operation that restores the natural state of the stomach, as well as putting a magnetic bracelet on the esophagus that prevents the reflux of acid masses.
Folk remedies
For the treatment of reflux with folk remedies, it is recommended to use decoctions and infusions from plant materials.
A teaspoon of crushed dill seeds, brewed with boiling water, effectively eliminates heartburn and stops inflammation in the esophagus.
During the day, you should take decoctions from herbal preparations from the rhizomes of the highlander, leaves of plantain, yarrow, oregano and chamomile. Before going to bed, teas from mint leaves, fireweed, calendula flowers and calamus root are shown for use.
The rule of preparing decoctions is to fill one tablespoon of the plant mixture with a glass of boiling water and incubate in a water bath for 15 minutes.
Diet for the disease
Clinical nutrition is designed to eliminate foods from the diet that have an irritating effect on the mucosa, as well as contribute to increased production of gastric secretion.

Good results are brought by the diet for reflux esophagitis, which includes such products:
- soft-boiled eggs;
- skim milk products;
- liquid and semi-liquid cereals;
- steam fish and meat;
- baked apples;
- white bread crackers.
Under the ban - coffee, alcohol, soda, any sour drinks, beans and peas, spicy, fried, smoked and salty dishes, chocolate and brown bread.
Prevention
The correct way of life is of great importance for recovery and prevention of recurrence of reflux. Patients are advised to maintain physical activity, monitor weight, not overeat, and after eating, take walks in the fresh air.
In addition, any load on the stomach should be excluded, including tight clothing and tight belts. Slopes after eating are not allowed. The head of the bed for night rest must be raised by 10-15 cm.
And most importantly - you need to regularly visit a gastroenterologist and promptly undergo all the prescribed examinations.












