It is difficult to maintain a healthy digestive system without knowing the location and functionality of its organs. Understanding what the pancreas is, where it is and how it hurts, allows you to pay attention to deviations in the gastrointestinal tract in time and prevent the development of severe, and often life-threatening, pathologies.
Material Content:
Where is the pancreas in humans?
The pancreas is called the digestive organ, which ensures the production of gastric juice and enzymes necessary for digestion.
The secretion produced by iron is involved in the processing of fats and proteins. Also, the endocrine glands located in the islet cells of the body synthesize insulin and glucagon - hormonal substances responsible for the metabolism of carbohydrates and the regulation of blood glucose levels.
The pancreas is a lobed formation of an elongated shape, from 16 to 23 cm in size. In the structure of the organ, the head, body and tail are distinguished.
The gland is located behind the stomach, close to the duodenum and is connected to it by ducts. When a person takes a lying position, the gland is below the stomach, hence its name.
The central part of the pancreas is closed by the stomach and is located at the level of the first lumbar vertebra. The caudal part of the organ is located on the left under the ribs and is in contact with the spleen.
The body of the gland consists of alveolar-tubular tissue with a huge number of ducts, blood vessels and nerves. From above, the organ is completely covered with connective tissue.
Organ functionality
The structure of the organ involves two functional components - exocrine and endocrine. In the exocrine part, digestive secretion is produced - the enzymes amylase, lipase and protease.
In the endocrine section of the pancreas, there are pancreatic islets - clusters of hormone-producing cells that produce:
- glucagon, which increases blood glucose;
- blood glucose lowering insulin;
- hypothalamic hormone somatostatin;
- pancreatic polypeptide that suppresses the secretion of the pancreas and stimulates the secretion of gastric juice;
- ghrelin secreted by epsilon cells to stimulate hunger.
Thus, the pancreas provides many vital processes for the human body. Even minor violations in the work of the gland entail the development of dysfunctions of other digestive organs.
How does the pancreas hurt?
A healthy person may not know where the pancreas is located - characteristic soreness is manifested only in case of impaired organ functionality. The development of pathological processes is indicated by the appearance after eating of pain in the left side of the hypochondrium, as it intensifies, covering the entire side and part of the back.
The pain syndrome may be accompanied by a feeling of fullness in the region of the ribs, which impedes normal breathing, which indicates an increase in the size of the pancreas.
As a rule, taking antispasmodic drugs at the time of the attack does not give a result, a slight decrease in pain occurs if you take a sitting position and lean forward.
The localization of pain symptoms indicates the defeat of a certain area of the pancreas. If pain occurs at a level between the left costal arch and the navel, this is a sign of inflammation in the tail of the gland. The appearance of pain in the area between the right costal arch and the navel indicates inflammatory processes in the head of the gland.
Symptoms and signs of organ pathologies
Pancreatic dysfunction is accompanied by a number of characteristic symptoms.
In addition to severe acute pain, the following are observed in patients:
- bouts of vomiting, frequent with increased pain;
- gastrointestinal problems - nausea, heartburn, belching, flatulence, rumbling in the abdomen, diarrhea;
- lack of appetite;
- temperature rise;
- yellowness of the sclera and skin;
- sweating
- tachycardia;
- rapid weight loss;
- general weakness.
Attacks of vomiting are considered the primary symptom of pancreatic pathologies. Arising in the morning or after eating, vomiting often precedes the development of pain. The appearance of vomiting with a bitter or sour taste is facilitated by gastric spasm. As a rule, after the release of vomit, the patient feels relief.
The severity of symptoms of pancreatic dysfunction is determined by the degree of development of pathological disorders.
The relationship of symptoms with the nature of the lesion of the gland
A decrease in pancreatic functional capacity immediately affects the quality of digestion processes.
The lack of lipase is evidenced by a change in color and consistency of feces. As a result of excess withdrawal of fatty substances, feces becomes yellow or orange and may have an oily appearance.
Amylase deficiency is expressed in violation of the absorption process of foods rich in carbohydrates. In this case, the stool becomes loose and watery, and its volumes exceed the usual level.
Trypsin deficiency leads to an increase in the amount of nitrogen compounds in the feces. Feces become mushy and contain undigested protein fibers. Differs in stench. May cause anemia.
Least of all, the lack of glucagon production is reflected in the state of the body - if necessary, the lack of glucose in the blood is compensated by the adrenal glands.
Pathological effects of individual symptoms
Against the background of disruption of food splitting processes, the body has a shortage of microelements and vitamins - a sick person has hair loss, dry skin, weight loss, brittle nails.
Undigested food fragments, entering the large intestine, provoke gas formation and frequent bowel movements.

The impaired functionality of hormone-producing islet cells is expressed in a decrease in insulin levels and the development of the initial stage of diabetes.
If there is a violation of the outflow of enzymes from the pancreas, the gland tissues are irritated and swell. With prolonged stagnation of enzymes in the organ, tissue necrosis begins.
Read also: how the pancreas hurts in humans
What diseases does pain indicate?
The appearance of a pain syndrome in the pancreas is always a sign of disorders leading to the development of serious diseases.

As the functionality of the organ decreases, pathological processes occur that accompany such diseases:
- pancreatitis - inflammation of the gland tissue. It is accompanied by the accumulation and activation of enzymes secreted by the iron, which leads to its destruction (self-digestion). In this case, substances are released that, entering the blood, damage the tissues of other organs - the heart, liver, kidneys, lungs and brain;
- abscess - One of the complications of pancreatitis caused by excessive drinking. It is characterized by the accumulation of dead tissue of the gland and their subsequent suppuration;
- pancreatic necrosis - A consequence of the acute form of pancreatitis. Accompanied by cell necrosis. May cause abdominal bleeding;
- chronic splenic vein thrombosis - The result of the development of pancreatitis. Accompanied by vomiting with blood and severe pain. It leads to an increase in the size of the spleen and a decrease in the body's defenses;
- cholestasis - a complication of the chronic form of pancreatitis. It is characterized by a violation of biliary processes and stagnation of bile;
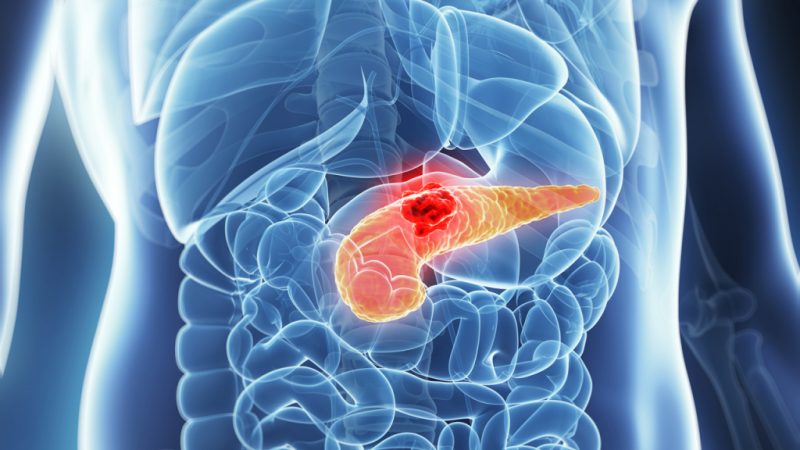
- pancreatic cancer - the development of malignant tumors in the epithelial areas of the glandular tissue and ducts. May appear against the background of diabetes mellitus, chronic pancreatitis and pancreatic adenoma;
- diabetes - develops against a background of insulin deficiency, which leads to impaired glucose processing and an excessive increase in its amount in the blood (hyperglycemia). It is accompanied by damage to the nervous, muscle, respiratory, immune, cardiovascular and reproductive systems.
Any diseases caused by pancreatic dysfunction pose a serious danger not only to the functionality of the digestive system, but also to human life.
What to do if the pancreas hurts?
Pathologies of the pancreas are most often accompanied by acute pain. Sick people and their loved ones need to know what to do if the pancreas hurts - timely medical treatment will help relieve pain and stop the further development of the attack. Then you should consult a doctor as soon as possible.

In the acute form of pancreatitis, the process can be stopped with the help of an ice compress applied to the pain localization site. For this, it is necessary that the sick person takes a lying position on a flat surface and relaxes. Tension of the abdominal muscles increases pain.
At the time of the attack, it is strictly forbidden to eat food, drinks and painkillers.
Patients with a diagnosed chronic form of pancreatitis are recommended to take painkillers prescribed by their doctor.
Diagnostic measures
To identify the cause of acute pain, doctors conduct an examination of the patient, especially paying attention to:
- the nature and localization of the pain syndrome;
- skin color and sclera;
- the severity of pain on palpation in the position of the patient lying on his back.
If pancreatic diseases are suspected, gastroenterologists prescribe laboratory tests to determine blood counts such as glucose, trypsin and amylase concentrations, white blood cell counts, liver enzyme activity, and bilirubin levels.

A urinalysis is prescribed to determine amylase. Fecal analysis helps to identify high fat, as well as chymotrypsin and trypsin.
Among the most informative instrumental diagnostic methods are ultrasound and computed tomography. The use of ultrasound allows you to evaluate the size of the pancreas, as well as detect the affected areas and the presence of cysts.
A study through computed tomography makes it possible to study the state of the pancreas and ducts. Also, for examining the ductal system of the gland, the method of cholangiopancreatography is used - the combination of endoscopy and radiography.
Diet for diseases
The basis of any therapeutic effect on the pancreas is a strict diet. The basis of dietary nutrition is the exclusion from the diet of products that irritate the gland or affect its functionality.

Prohibited:
- any types of fatty foods:
- alcohol and smoking;
- strong or saturated drinks;
- spicy dishes with spices, spices and seasonings;
- preservation;
- smoked meats;
- fried food;
- confectionery.
During an exacerbation of pancreatitis, eating is prohibited - for three days only water without gas or weak herbal teas are allowed.
At the end of the specified period, a gradual transition to medical nutrition begins - buckwheat with kefir, liquid semolina porridge on the water, steamed dishes, white meat of poultry and fish, low-fat cottage cheese, boiled vegetables, cereals, omelets, compotes and jelly.
Failure to comply with dietary rules reduces the effectiveness of drug therapy and negates the possibility of restoring health.












