Pneumocystis pneumonia is pneumonia caused by a conditionally pathogenic yeast-like fungus. The disease does not develop in animals, and is typical only for humans. Normally, in a healthy person, pneumocysts are also present in the lungs, but they can cause a pathological process only with a decrease in immunity.
Antimicrobial and antibacterial drugs are used for treatment, as well as drugs aimed at increasing the body's defenses. Delaying with therapy leads to the development of complications, for example, emphysema or fibrosis.
Material Content:
The incubation period and pathogens in children and adults
Pneumocystosis is an opportunistic infection, so its pathogens are always in the human body, but they begin to show their aggressiveness only under certain conditions. The microorganism belongs to the kingdom of mushrooms, but, despite this, the usual antimycotic drugs in the fight against it are ineffective. It is not possible to grow a pneumocyst in artificial conditions (cultivate), which significantly complicates the study of the microbe.
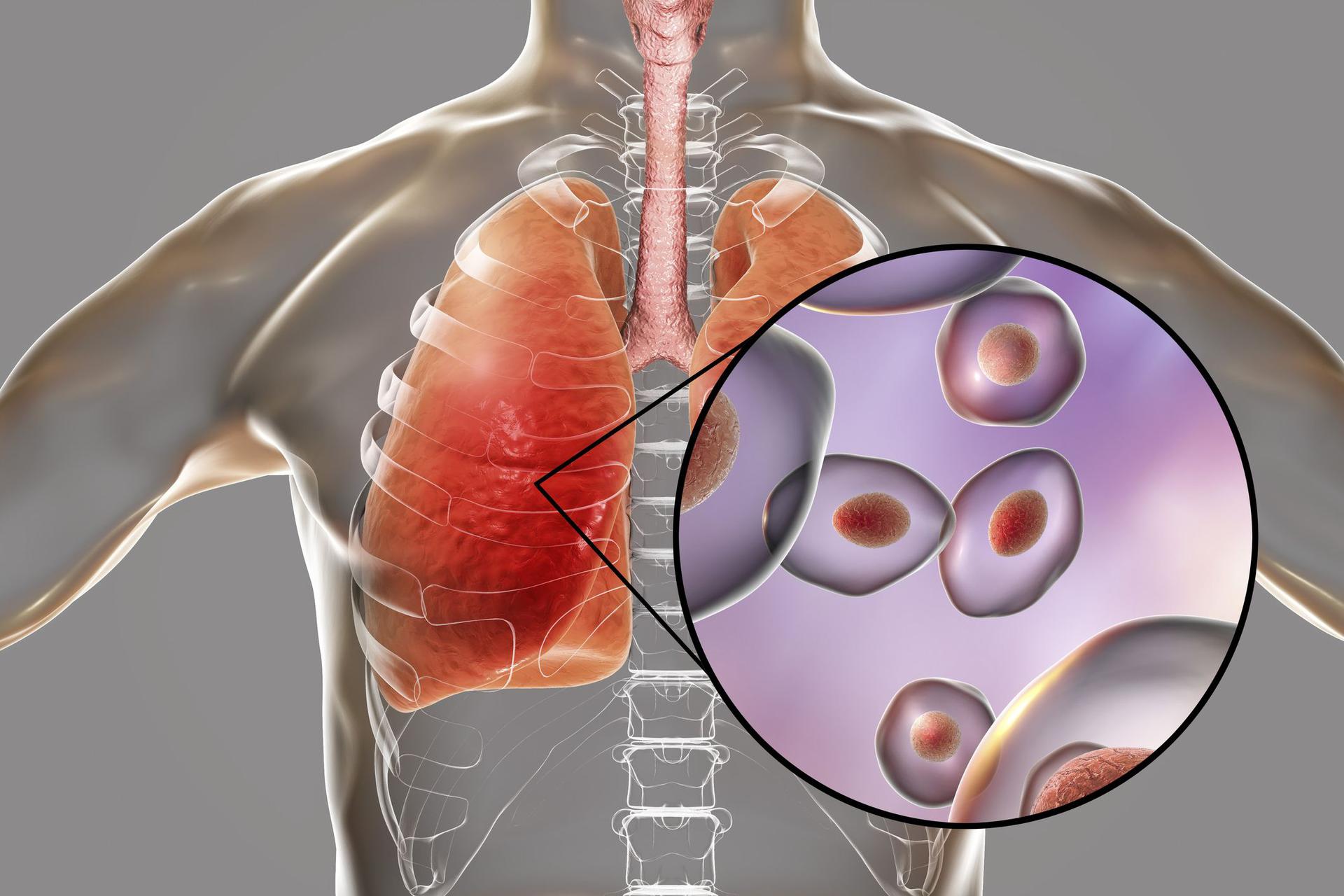
In the life cycle of Pneumocystis jirovecii, there are three stages:
- trophozoite - an amoeboid mononuclear microorganism having several vacuoles;
- precyst - an intermediate stage;
- cysts are spherical cells with a thick cell wall.
The causative agent does not parasitize inside the cells; asexual and sexual reproduction are alternately replaced in its cycle.
The incubation period of pneumocystis lasts from 7 to 10 days. At this time, they actively multiply, but do not cause any clinical changes in the human body. In patients with a sharply reduced immune response, the latent phase of the disease can be shortened by several days. This often happens in people with AIDS, in the presence of malignant tumors, or in those taking immunosuppressive therapy. Also, premature babies under six months of age are prone to the accelerated development of the disease.
Symptoms and signs of pneumocystis pneumonia
Symptoms of pneumocystis pneumonia begin to appear a week after the activation of pathogens in the body. During the disease, three stages are distinguished - edema, atelectasis, emphysema:
- The duration of the first is 7-10 days. The infection is only gaining strength, so the signs of pathology are mild. The temperature is kept within normal limits, sometimes rising to subfebrile condition (37-37.5 ° С). The patient develops weakness, decreases working capacity, and appetite worsens. In certain cases, weight loss is possible. A dry cough periodically appears, during which a small amount of viscous sputum is secreted.
During auscultation, hard breathing is heard in the lungs, but there are no rales. The percussion sound is shortened in the interscapular region. - After a week, the disease passes to the second stage, which lasts up to one month. The patient complains of shortness of breath, which increases over time. Coughing attacks are becoming more frequent, it becomes intrusive. The nature of sputum changes - they become thicker, more difficult to depart.
At a medical examination, cyanosis of the skin and participation in the breathing act of additional muscles are noticeable. Small and medium bubble rales appear in the auscultatory picture. Perhaps the development of respiratory failure. - The last stage of pneumocystosis lasts 1-3 weeks. The patient's well-being is gradually improving: the number of seizures decreases, the cough becomes less intrusive, sputum liquefies, and breathing problems disappear. Auscultatory and percussion changes persist for a long time.
Symptoms of pneumocystis pneumonia are also characteristic of other types of pneumonia. To prove the presence of a pneumocyst in the body, you need to resort to additional methods of examining the patient's condition and the presence of a pathological process.
Diagnostic Methods
If it is suspected that the lung tissue is affected by pneumocysts, the specialist will first of all recognize the epidemiological history. This helps to understand whether the patient belongs to a risk group, and what is the likelihood of having precisely pneumocystosis. It is important for the attending physician to determine:
- whether the patient was in contact with a person sick with this disease;
- the presence of HIV infection or AIDS;
- taking medications that reduce the body's resistance (immunosuppressants);
- the presence of other problems causing immunodeficiency.
To prove or disprove the development of this disease in the body, the doctor prescribes a number of additional studies:
- blood test - signs of inflammation are visible (SHO acceleration, a large number of white blood cells), hemoglobin decreases due to respiratory failure;
- analysis for parasites - a microscopic examination of secretions to identify a pneumocyst in them;
- blood serology - the presence of specific antibodies;
- X-ray - vascular pattern is amplified, shadows are visible (lesions), areas of pathological transparency.
Timely diagnosis allows you to quickly start treatment and minimize the degree of consequences of the disease. At the first symptoms, you need to seek specialized help and do not self-medicate.
Features of the course of the disease in HIV-infected
Pneumocystis pneumonia in HIV-infected people is the most common opportunistic infection.Due to a sharp decrease in the body's defenses, the ailment causes severe intoxication, takes a long time and is prone to chronicization of the inflammatory process. The incubation period is shortened, almost 100% of cases end with complications. In addition, in 60% of cases, pneumocytosis recurs after a short period of time.
Treatment of pneumocystis pneumonia
Therapy of the disease should be carried out strictly in a hospital under round-the-clock medical supervision. In addition, a separate sterile ward with laminar air flow is allocated to HIV-infected patients and premature babies. Treatment lasts from two weeks to a month, during the entire period of time the patient should be in the hospital.
With the timely and correct use of medicines, 80–90% of the initially ill survive. In re-infected, the survival rate is reduced to 60%.
Traditional treatment
The main drugs for the treatment of pneumocystis pneumonia are antibiotics and antimycotic drugs. Doctors prescribe several different types of tablets, which you need to take according to the scheme. To improve the general well-being of the patient and maintain the strength of the body, medications of certain groups are prescribed:
- antiretroviral - only for HIV-infected people;
- anti-inflammatory;
- expectorant;
- antipyretics (against temperature);
- mucolytics;
- probiotics;
- hepatoprotectors.
Following all the instructions of the attending physician, the patient always manages to recover and, most likely, to avoid complications.
Folk remedies
Alternative methods of treatment are not able to withstand pneumocystosis, they can only be used as maintenance therapy. Various teas, tinctures, lotions, inhalations and natural ointments help relieve sputum, lower body temperature, support immunity. The most effective recipes are considered using these ingredients:
- warm milk with honey;
- ginger, fig;
- garlic, black radish;
- decoctions and tinctures of sage, marshmallow;
- linden tea;
- raspberry jam, grated with sugar viburnum.
Before starting an alternative treatment, it is recommended to consult with your doctor to make sure there are no contraindications.
Consequences and preventive measures
Without proper preventive measures, pneumocystis pneumonia re-develops over the course of a year in more than half of those who are ill. Therefore, after the transferred pathology, a course of special drugs should be taken. For the same purposes, it is necessary to undergo chemotherapy in the presence of the following conditions:
- changes in blood composition - low percentage of CD4 lymphocytes;
- oral candidiasis, which is accompanied by severe intoxication and fever;
- prolonged use of immunosuppressants, for example, during organ transplants;
- a significant decrease in the body's defenses;
- the presence of HIV infection or malignant tumors.
Pneumocystosis is dangerous for the development of complications that can occur even with the correct and timely treatment. The most susceptible to the manifestation of negative consequences are weakened categories of patients - HIV-infected and elderly people. The disease is also dangerous for premature babies in the first months of life, especially if the baby has underdeveloped lungs.
Possible complications:
- abscess (abscess);
- gangrene (necrosis and decay of the lung tissue);
- catarrhal or purulent pleurisy;
- pneumothorax (air entering the lungs);
- emphysema (destruction of the structure of the alveoli);
- acute and chronic respiratory failure.
Strengthening immunity will help minimize the possibility of pneumocystosis and the development of complications: exercise, hardening, proper nutrition. People at risk should periodically undergo chemoprophylaxis.