Many people are not inclined to heed medical warnings about the consequences of a frivolous attitude to their health. And in vain. Because microorganisms such as mycoplasma pneumonia are just waiting for the right moment to attack the body.
Worst of all, at the first stage of development, an infectious lesion looks like an ordinary cold. And since the possibility of determining the exact diagnosis appears a week after infection, patients can not always immediately receive adequate treatment.
Material Content:
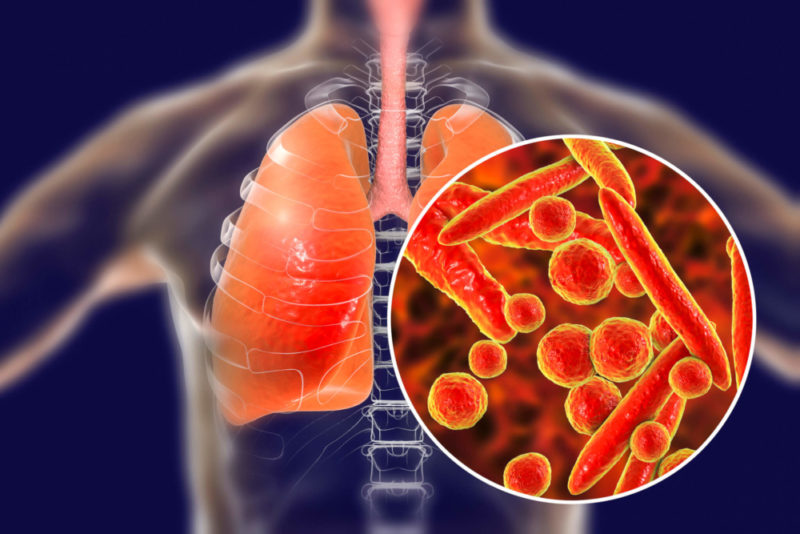
What is the bacterium mycoplasma pneumonia?
Despite the achievements of medicine in the prevention of epidemics, outbreaks of lesions of mycoplasma infection are still marked by a clear frequency of 5-8 years.
Mycoplasmosis is the result of damage to the body by bacteria of the genus Mycoplasma. This microorganism is characterized by the absence of a cell wall and the need for free oxygen. The absence of a membrane in the cell is compensated by a three-layer cytoplasmic membrane, which provides bacteria with resistance to antibiotic agents.
In addition, mycoplasma simultaneously possesses the properties of both bacteria and viruses, and can not only be in the human body for a long time without manifesting itself, but also integrate into its genomes.
The development of an infection in which the respiratory tract is affected is the result of localization in the respiratory organs of the smallest representatives of the Mycoplasma class, unicellular obligate bacteria of the gram-negative type - M. pneumoniae.
Mycoplasma does not just parasitize on red blood cells and cells of the ciliary epithelium of the bronchial tree. Introducing into the cells, bacteria absorb nutrients, releasing harmful metabolic products.
In this case, the pathogen skillfully disguises itself as an antigenic composition of cells, thereby provoking the appearance of autoimmune reactions. Indeed, the cells in which the bacterium has “settled” are perceived by the human body as foreign.
Such processes affect the nature of symptomatic manifestations and significantly complicate the diagnosis of infection.
The causative agent of which diseases is
Mycoplasmas penetrate the human body by airborne droplets - through the nasal passages. They are fixed on the cells of the mucous membrane of the organs of the respiratory system - bronchi, trachea, lungs.
As pathogenic microorganisms multiply, the process of inflammation of the mucous membrane of the respiratory organs intensifies and tonsillitis, pharyngitis, tracheobronchitis, and mild SARS develop.
And in the transition to a chronic course - pneumosclerosis, bronchiectasis and bronchial asthma, as well as exudative or fibrinous pleurisy.
Usually, respiratory mycoplasmosis occurs seasonally, in the cold season, when people spend a lot of time indoors. Vitamin deficiency and stress contribute to weakened immunity and reduce the body's resistance to infections.
Symptoms of mycoplasmosis in children and adults
The first symptoms of mycoplasma damage are manifested not only in the form of a respiratory syndrome, but also as signs of extrapulmonary lesions. And since the incubation period lasts from two to four weeks, the increase in symptoms occurs gradually. The acute form of manifestations of mycoplasma pneumonia is less common.
The duration of the incubation period depends on the state of the human immune system and the number of pathogens that have entered the body.
In most cases, mycoplasma damage manifests itself in the form of:
- dry nasopharyngeal mucosa;
- protracted paroxysmal unproductive cough;
- chest pain, aggravated by inhalation and exhalation;
- dry wheezing;
- headaches;
- redness of the throat;
- a slight increase in temperature to 37.7 ° C. In the acute course of infection, on the 5-7th day, the temperature can rise to 40 ° C;
- general weakness and pain in the joints.
As additional symptoms are considered: digestive problems, skin rashes, abnormalities in the liver, kidneys, heart, brain, changes in blood analysis, up to anemia.
In the absence of a secondary microbial process and other complications, the severity of symptoms of mycoplasma pneumonia gradually fades over ten days.
It is characteristic that the development of symptoms can be caused not only by the progress of the infection, but also by the autoimmune reaction of the body caused by it.
Immunoglobulins - antibodies that the body of an infected person produces in response to a bacterial lesion, can destroy the tissues of any organs.
Diagnostic measures
Diagnosis is possible only after complete identification of the causative agent of the infection. Diagnosis of the disease is simplified if there is information that infected people are in the patient’s environment.
In all other cases, a diagnosis can be made using laboratory tests and only after a week after the onset of symptoms.
The most effective diagnostic methods are:
- a general blood test allows you to draw conclusions about the quality of its composition. An increase in the number of leukocytes indicates inflammatory processes in the body and may be one of the possible signs of mycoplasmosis;
- ESR indicators. The increased erythrocyte sedimentation rate indicates not only the presence of inflammation, but also mycoplasma infection;
- enzyme immunoassay of venous blood. The determination in the blood of antibodies to Mycoplasma pneumoniae IgG or IgM in the presence of characteristic signs is regarded as confirmation of mycoplasma infection;
- roentgenogram - with mycoplasma, the pulmonary pattern is enhanced. In the lower parts of the lungs, lesions are observed - heterogeneous, with vague contours;
- inoculation on mycoplasma taken from the nasopharynx allows you to determine the level of sensitivity of the pathogen to various types of antibiotics;
- Ultrasound is a tool for visualizing structural changes in organs.
The choice and purpose of diagnostic studies is determined by the clinical picture of the disease.
Diagnostic features in the presence of immunoglobulins in the blood
In the first five days after the onset of symptoms of the disease, antibodies of the IgM type are formed in the blood of an infected person. Therefore, the analysis of Mycoplasma pneumoniae IgM made during this period can quite accurately determine the nature of the pathology.
A positive test result indicates the acute nature of the infection.
Whereas the determination of antibodies such as IgG in a blood test indicates a prolonged course of the disease.
Although this type of immunoglobulin does not appear in the blood immediately, but a few weeks after infection, it persists for a long time.
To correct diagnostic findings, it is recommended to do a second blood test in two weeks.
Treatment methods
Due to the intracellular cycle of mycoplasmosis development, the use of penicillins and other types of β-lactam antibiotics in the treatment of mycoplasmosis is considered inappropriate.
The optimal treatment result is achieved using drugs that can accumulate in the cells, thus blocking the activity of pathogens. Representatives of the macrolide group, azithromycin and clarithromycin, possess such properties.
The action of macrolides is based on their ability to penetrate into the affected cell and block the synthesis of protein necessary for the development and reproduction of the pathogen.
Advantages and disadvantages of antibiotic therapy of mycoplasmosis
The choice in favor of macrolides is due not only to a high level of their effectiveness.
But also the presence of advantages compared with other types of antimicrobial agents used to treat mycoplasma, in particular, fluoroquinolones and tetracyclines:
- slight toxicity;
- the creation of large concentrations of active substances in the affected tissues;
- safety in the treatment of pregnant women or children, including newborns;
- lack of side effects;
- prolonged antibacterial action due to the ability to cause irreversible changes in the ribosomes of bacteria.
The disadvantage of antibiotic therapy is its ability to affect only intracellular types of pathogen. While other morphological forms remain in the body, and under a combination of favorable circumstances, they can not only activate again, but also provoke the development of complications.
Therefore, along with antibiotic therapy, in the treatment of mycoplasma pneumonia, drugs that relieve symptoms are used - expectorant and antipyretic drugs, as well as immunomodulators and other types of drugs that provide correction of the immune response.
In the acute course of mycoplasmal pneumonia, inpatient treatment, strict bed rest, a diet rich in protein, and an abundant intake of fluids with plant extracts (juices, fruit drinks, compotes from cranberries, currants and rose hips) are prescribed.
The pronounced effect of therapy with mycoplasmosis is observed on the third day of intensive treatment.
Forecast and Prevention
Mycoplasmal types of pneumonia most often affect people with a weakened body - children, adolescents, young people under the age of 30 years, the elderly.
In the absence of complications, the prognosis of the disease is favorable, despite the fact that the affected areas of the lung tissue may remain sclerosed.
With the development of complications, the prognosis worsens, since severe pathological processes can threaten the patient's life.
The main cause of infection is a long stay in closed rooms with a large number of people (possibly infected) against a background of weak immunity and a lack of vitamins in the body. Therefore, the most effective way to prevent infections or their relapses is considered stable support of the body, aimed at strengthening the immune system.
Most pulmonologists are inclined to a complex effect on internal organs and systems, as well as compliance with standard measures of a healthy lifestyle:
- giving up bad habits;
- good nutrition with a predominance of protein foods and vegetables;
- regular exercise;
- hand hygiene;
- walks in the fresh air;
- physiotherapeutic procedures;
- massage effects;
- respiratory gymnastics.
Among the additional measures to enhance the protective properties of the body - spa treatment in institutions located in areas with a dry but warm climate or in the mountains.
A full course of adequate treatment and the observance of preventive measures are the most effective ways to prevent re-infection of mycoplasma pneumonia and the transition of the disease into a chronic form.
Extrapulmonary complications of mycoplasmosis
The development of mycoplasma infection is characterized by a simple course and is visually identified when there are pronounced signs of intoxication of the upper respiratory tract.
At the initial examination, the therapist can not always get enough data for a differential diagnosis, since not only the primary signs, but also the results of laboratory tests indicate diseases like ARI.
For this reason, even experienced doctors can not always differentiate mycoplasma pneumonia from viral lung lesions.
Aggressive activity of Mycoplasma pneumoniae in weakened organisms leads to non-respiratory lesions and causes dysfunctions not only of the respiratory system, but also of other internal organs.
In the absence of timely or adequate treatment, the infection can invade the tissues of the heart system or brain.
Chronic exposure to pathogenic cells leads to the development of:
- aseptic meningitis;
- meningoencephalitis;
- pericarditis;
- myocarditis;
- neurological complications;
- hemolysis;
- exanthema;
- arthritic lesions;
- liver dysfunctions;
- inflammation in the tissues of the pancreas;
- pathologies of the eye.
The only distributor of mycoplasma infection is considered to be a person, and only an organism with weakened immune defense can be the most vulnerable object for pathogens.
Therefore, there is only one way to avoid damage by the mycoplasma bacterium - a healthy lifestyle and careful attention to the health of your body.