The most dangerous infectious diseases lie in wait for those people who do not care about their health. Most patients with inflammation of the membranes of the brain and spinal cord not only did not know how meningitis is transmitted, but they were sure that this disease was the result of hypothermia, not infection.
To avoid a difficult pathological process, it is necessary to understand how the transmission and development of the disease occurs, as well as adhere to the rules of its prevention.
Material Content:
Routes of transmission of infection in children and adults
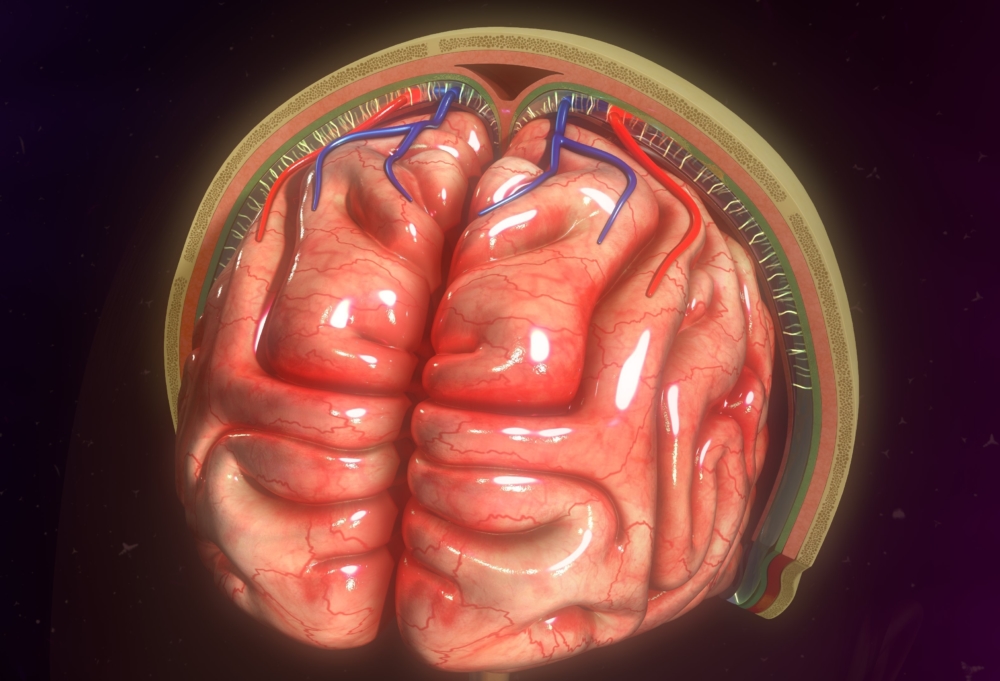
The human brain is protected immediately by three shells - hard, arachnoid and soft. When pathogens or viral particles enter the body, the infection enters the bloodstream and spreads to all tissues, including the brain.
Having reached the brain, pathogens encounter an obstacle - protective membranes, affect them and begin to multiply actively. The life processes of microbes cause inflammation, which in medicine is called meningitis.
It can be caused by viruses, bacteria, fungi or parasitic cells. Accordingly, there are different ways of infection with the infection:
- airborne. Infected people often sneeze and cough, spreading many pathogenic microorganisms around themselves.To get infected by airborne droplets, it is enough to be near a sick person without a mask covering the nose and mouth;
- contact. Some types of meningitis pathogens can be released into the biological environment of an infected person or on the surface of his mucous membranes. In such cases, the transmission of infection occurs in contact with areas in which the pathogen is located. This happens during a handshake, kiss, hug, or through hygiene items, personal items, toys, household appliances;
- fecal-oral. One of the most common mechanisms of infection with meningitis, in which the pathogen enters the body along with contamination through hands, food, water. Infection occurs when eating unwashed vegetables and fruits, swallowing water in ponds or conscious ingestion of fluid from unverified sources. Dirty hands are also considered one of the possible ways for viruses to enter;
- transmissible. Provides for the participation of an intermediary - an insect carrier of infection;
- transplacental - that is, the intrauterine route of infection with meningitis, in which the fetus becomes infected by the infection from the mother during pregnancy or during childbirth.
Having penetrated the body, the causative agents of meningitis enter the blood and lymph, getting the opportunity to transport to all tissues and organs.
In the absence of favorable conditions for reproduction and vital activity, some types of pathogens of infection can become latent. Such pathogens are able to stay in the body for a long time without manifesting anything, and become active after months and even years with a decrease in the functionality of the immune system.
Classification of the disease by the type of pathogen
Meningitis is classified according to the type of pathogen that affects the meninges. The etiology of the disease is determined by the following types of lesions:
- bacterial. Pathogens - pneumococci, tuberculous mycobacteria, meningococci, hemophilic bacillus;
- viral. Pathogens - enteroviruses, human herpes virus, lymphocytic choriomeningitis virus;
- fungal. The causative agents are cryptococci, candida, coccidia;
- protozoal. The causative agents are toxoplasma, malarial plasmodium, amoeba.
A bacterial lesion is characterized by a purulent inflammatory process and is accompanied by neutrophilic pleocytosis. All other types of pathogens cause serous meningitis, in which the number of lymphocytes in the cerebrospinal fluid increases.
How to recognize an ailment by the first signs
The first signs of the disease with different types of disease may vary.
Acute forms of pathology are characteristic of meningococcal, secondary purulent and viral meningitis. Suddenly, a fever appears in the form of severe tremors and chills, then the temperature rises sharply and an intolerable headache appears.
With tuberculous, protozoal and serous meningitis, the disease manifests itself gradually starting with a subtle deterioration in well-being and loss of appetite. As the pathology develops, the severity of its symptoms also increases, until the symptoms peak in the onset of the acute phase.
Nevertheless, infectious meningitis of any etiology can be recognized by signs characteristic only for this disease:
- high temperature, which is difficult to bring down with the help of traditional means;
- severe headaches that are not amenable to analgesic relief;
- double vision, sensitivity to light;
- nausea and vomiting in the absence of appetite;
- the occipital muscles lose their flexibility and become hard, because the head is fixed in a thrown back state. It becomes extremely difficult to straighten the neck;
- when trying to bend the neck and move your head forward, the leg bends at the knee;
- if you raise your leg up, it becomes impossible to bend it at the knee;
- the appearance of a rash, the color of which does not lose brightness even when you press the skin;
- in infants - fontanel swelling.
All these signs indicate the presence of meningeal syndrome - an alarming signal about the possible development of infectious meningitis. The patient is put to bed, dim the light, provide maximum peace and immediately call a doctor.
Symptoms and clinical presentation
Each type of meningitis has its own characteristics of development, clinical manifestations and the nature of tissue damage.
Bacterial meningitis
In adults, the disease makes its debut with repeated vomiting amid a sharp increase in temperature and severe headache. On the first day, a rash of erimatous or measles-like character appears.
The back wall of the nasopharynx swells, the tissue structures of the follicles noticeably increase in size.
Severe forms of pathology are accompanied by dimming of consciousness, delirium, cramps, paralysis of the eye muscles, tissue necrosis, damage to the cranial nerves and strabismus. If meningococcal meningitis becomes negative, the patient may die without regaining consciousness.
With a favorable course of the disease, improvement occurs in a week, and full recovery - in a month and a half.
In infants, the development of bacterial meningitis occurs gradually.
Secondary bacterial meningitis manifests itself in a purulent form and is characterized by an acute course. It is accompanied by pronounced meningeal syndrome.
Serous meningitis
In most cases, serous meningitis is observed in children aged three to six years. Adults and schoolchildren suffer much less often.
The acute phase of the pathology is preceded by a two-week prodromal period, during which the first symptoms of the disease may appear - a slight increase in temperature, poor health and loss of appetite.
At the end of the prodromal period, the disease takes on an acute form, which is characterized by all the components of the meningeal syndrome.
Tuberculous meningitis
Meningeal symptoms occur two weeks after the first symptoms of a general deterioration in well-being. Strengthening the clinical picture occurs gradually. May be accompanied by seizures and loss of consciousness.
Viral meningitis
It always starts immediately with the acute form, which is preceded by two days of the incubation period. Signs of intoxication and meningeal syndrome appear on the first day of the disease. In addition, symptoms characteristic of viral infections are observed - a runny nose, cough and sore throat.
Normalization of temperature and improvement of well-being occurs after four days. The full recovery period depends on the type of virus and can range from two weeks to several months.
Fungal meningitis
It begins with a subacute form, which gradually becomes chronic. It is accompanied by lethargy, drowsiness, anxiety and impaired consciousness of the patient. In most cases, a low temperature is observed. Meningeal syndrome is mild or completely absent.
Severe forms of fungal meningitis cause cerebral edema and can cause coma and death.
Protozoal meningitis
One of the rare forms of meningitis. The development of protozoan meningitis occurs against the background of a decrease in immunity and activation of the pathogen, which was in an inactive state in the body.
The main symptoms are severe meningeal syndrome, muscle pain, enlarged lymph nodes, joint pain, periodic chills, inflammation of the retina, choroid and iris.
Diagnostic measures
Meningitis refers to diseases whose diagnosis and treatment are the responsibility of a neurologist.
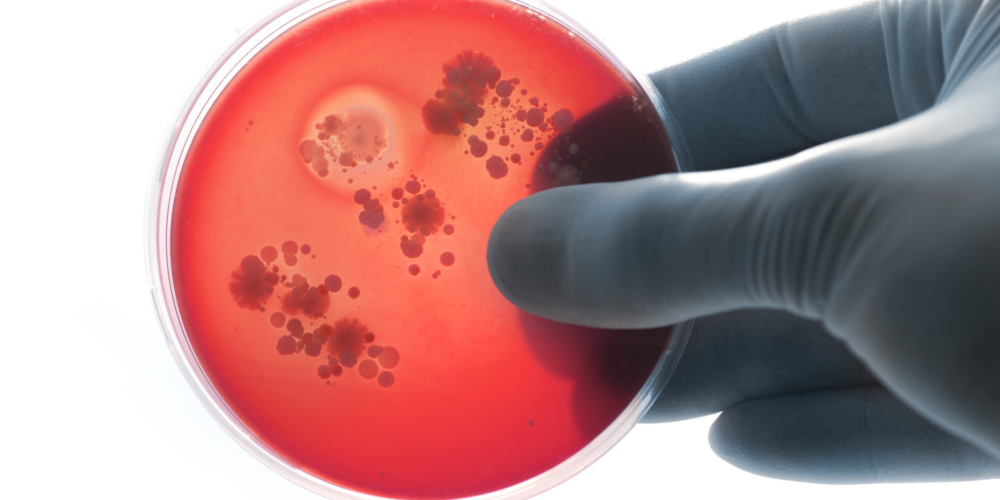
The initial detection of the disease is based on a physical examination of the patient and the presence of meningeal symptoms. To confirm the diagnosis, methods are used to determine the presence of the pathogen in the biological environment of a person - lumbar puncture and PCR.
Doctors obtain additional diagnostic information through laboratory tests of the patient’s blood, feces and urine.
Various changes in the uniform composition of the blood are regarded as a sign of a particular type of disease:
- the predominance of lymphocytes, a decrease in glucose levels - a serous viral or fungal infection;
- the predominance of neutrophils, a decrease in protein, up to a complete absence - purulent-bacterial disease;
- an increase in the number of protein and lymphocytes, leukocytosis - a tuberculous form.
To determine as accurately as possible what type of pathogen caused inflammation of the meninges, neurologists analyze and compare the characteristics of all studies.
Particular attention is paid to indicators characterizing the state of cerebrospinal fluid - its color and transparency, pressure level, leakage rate at the time of puncture, as well as cytosis data.
If differentiation is necessary, additional diagnostic tests are prescribed - CT, MRI.
Preventive measures
Preventive measures to prevent the development of meningitis are the general strengthening of the body and the elimination of provoking factors.
Effective prevention of meningitis includes the following measures:
- temper with water treatments and sports;
- vaccinate against pathogens or pathogens that provoke its development;
- observe hygiene rules;
- avoid contact with infected people;
- refrain from swimming in ponds;
- take care of your health, provide timely therapy for any inflammatory processes;
- take immunomodulatory drugs;
- organize a healthy diet and lifestyle.
Infectious pathologies lie in wait for those who are careless about the state of their body. Health promotion is a simple way not only to life without disease, but also to longevity.