Modern medicine can prevent many diseases, including measles, smallpox, polio, which previously caused epidemics and thousands of deaths. Today, a simple injection with a vaccine avoids chronic liver diseases, in particular, hepatitis D can be prevented by timely vaccination. This is a serious ailment that, without proper treatment, can cause acute liver failure in the shortest possible time.
Material Content:
What is viral hepatitis D
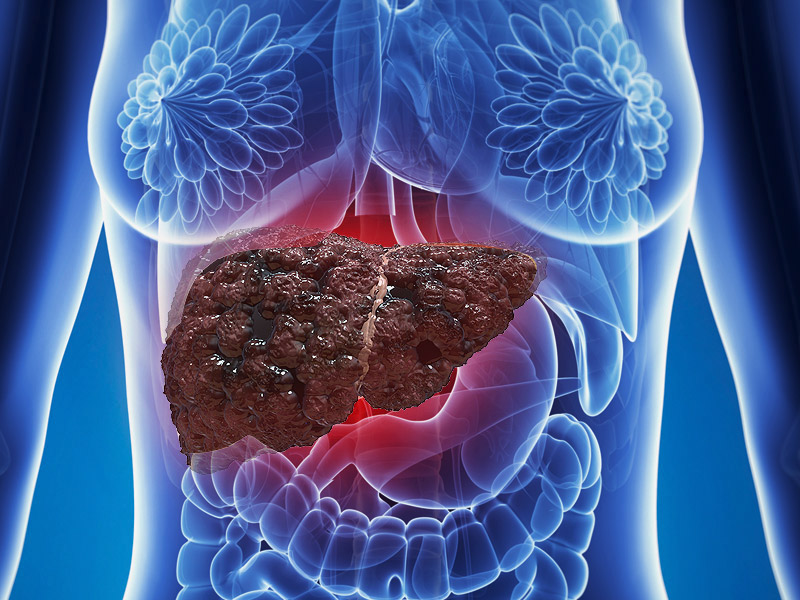
Viral hepatitis D or delta hepatitis is a chronic liver disease that occurs when the causative agent of Hepatitis deltavirus (HDV) is present and is a companion disease of hepatitis B. In the human body, type B hepatitis begins to develop along with type D (co-infection) or the second genotype of the virus begins to act a little later, and provokes the occurrence of superinfection. In any case, the carrier of two genotypes at once has an accelerated damage to the liver cells, which leads to its rapid death in the process of developed cirrhosis or oncological tumors. Among all genotypes, species D is one of the most dangerous - the mortality rate is 20%.
 Hepatitis D cannot progress in the body on its own - for this, it needs a virus of type B. Deltavirus itself is similar to plant molecules and is a satellite, that is, it cannot develop in healthy cells. It is believed that deltavirus simply uses the envelope proteins of the genotype B virus. When it enters the bloodstream, it provokes a reaction of the immune system that attacks the liver.
Hepatitis D cannot progress in the body on its own - for this, it needs a virus of type B. Deltavirus itself is similar to plant molecules and is a satellite, that is, it cannot develop in healthy cells. It is believed that deltavirus simply uses the envelope proteins of the genotype B virus. When it enters the bloodstream, it provokes a reaction of the immune system that attacks the liver.
Developing in parallel, genotypes B and D are more pronounced than genotype C, however, they act much faster. Once in the cells, the virus causes the proteomes in the liver cells to change, which leads to tissue degeneration and the formation of malignant tumors. The most common outcome of this disease is liver carcinoma.
Causes and Risk Factors
The source of a viral infection is always the carrier of the virus, i.e., a patient with hepatitis B and D. Moreover, his ability to infect others varies depending on the viral load - the number of pathogen cells in the blood, but there is always a risk. The likelihood of infecting others increases with the transition of the disease to the acute phase.
Hepatitis D is transmitted in two ways - through the bloodstream and discharge during intercourse. The most likely method of infection is a blood transfusion from the carrier, because donor checks do not always establish the presence of a pathogen. About 0.01-2% of all donors are carriers of undetected hepatitis of various genotypes. In addition, there are a number of other possibilities to obtain the pathogen virus:
- surgical intervention;
- sexual contact with the carrier;
- invasive medical procedures;
- use of non-sanitized tools.
The pathogen penetrates the placental barrier, so there is a risk of infection in the womb, while the pathogen does not penetrate into breast milk. The following persons are at risk:
- Having chronic hepatitis B.
- They need a transfusion of blood or its preparations (especially with repeated procedures).
- Often visited by incompetent nail salons or self-taught masters.
- They inject drugs.
- They have a weakened immune system.
- Make tattoos in non-certified tattoo parlors.
- Abandoned hepatitis B vaccination.
- Residents of countries with high prevalence of HDV.
- Have erratic sexual intercourse without protection.
Studies have shown that about 40% of patients could not identify the path of their infection. Migration of people from countries with an increased incidence of hepatitis B also affects the epidemiological situation in host countries.
Symptoms and forms of the disease
Since genotype D develops against the background of existing hepatitis B, the symptoms of the disease intensify, manifesting in the early stages. Signs of hepatitis D and B are similar and similar to those of jaundice:
- weakness;
- constant fatigue;
- lack of appetite;
- pain in the stomach and liver;
- insomnia;
- nausea;
- yellowed skin;
- discoloration of urine and feces.
The first symptoms appear within 2-3 weeks after infection, depending on the strength of the patient's immunity. In hepatitis D, there are three forms of the course:

- Incubation is the time from the moment of infection to the onset of the disease. The period lasts about 21-50 days, is often asymptomatic (slight fatigue and lack of appetite are possible).
- Pre-icteric - at this time the first signs appear. The stage lasts 4-10 days, during which the person constantly gets tired, observes sharp jumps in body temperature and pain in the joints and muscles of the body. Most often, the preicteric form of hepatitis D proceeds without specific signs (yellowing of the skin or discoloration of the urine), so patients do not pay much attention to other ailments.
- Jaundice is a form of the heyday of the virus in the blood, which begins to proliferate and affect the liver. The patient's eyeballs and skin turn yellow, pains appear in the stomach and in the region of the liver, which becomes an occasion to contact a gastroenterologist who can identify the development of pathology. This happens 2-3 months after infection.
The icteric stage corresponds to the acute form of hepatitis D and ends either with the full recovery of the patient (with proper treatment), or the development of a chronic form of the disease.
Diagnosis
To determine whether a person suffers from hepatitis D, antibodies that generate immunity in response to an attack of the pathogen virus allow. As soon as the RNA of the pathogen enters the bloodstream, the immune system begins to produce anti-HDV - antigens that attack the pathogen molecules. After the patient visits the therapist or gastroenterologist, the diagnosis begins, which consists of several stages:

- Visual examination of the patient - examine the skin, carry out palpation of the liver. In parallel, the patient is questioned, determining whether he was vaccinated against hepatitis B, whether he is at risk, whether there were contacts with carriers.
- Biochemical blood test - detect the presence of anti-HBV, check the level of bilirubin, platelets, aminotransferase, etc.
- Analysis of the genotype of the virus - in the case of a positive biochemical study of the patient’s blood, it is necessary to determine the type of hepatitis in order to choose the most appropriate treatment.
- Ultrasound (CT or MRI) of internal organs - this study will allow the doctor to see the current state of the organ and determine the phase of the disease, as well as choose the right therapy.
- Liver biopsy - this analysis is carried out if the previous ones were not obvious and did not provide the necessary data.
The main criteria for diagnosis are specific virus markers (anti-HDV) and changes in blood biochemistry.
Hepatitis D Treatment
The methods of therapy depend on the detected form of hepatitis and the degree of liver damage. The acute form of the disease is treated stationary, because it requires an integrated approach. In this case, the medicines used are the same as for hepatitis B - alpha-interferon and its derivatives.
The main difference between hepatitis D is its high resistance to drugs, so interferon is not a mono-drug. Gastroenterologists with him apply:
- Enterosorbents (lactofiltrum).
- Hepatoprotectors (heptal).
- Antiviral drugs.
 The latter type of medicine is prescribed in stronger dosages than for patients with hepatitis B, due to the stability of the delta virus. In addition to these drugs, modern therapy also provides drugs that inhibit the action of the pathogen and prevent the connection of the RNA of the virus with the protein cells of the body.
The latter type of medicine is prescribed in stronger dosages than for patients with hepatitis B, due to the stability of the delta virus. In addition to these drugs, modern therapy also provides drugs that inhibit the action of the pathogen and prevent the connection of the RNA of the virus with the protein cells of the body.
The course of treatment is from 3 months to a year or more in the absence of a therapeutic effect. For some patients in the later stages of the development of the disease and with irreversible liver damage, an organ transplant option is being considered.
Diet for the disease
As a result of the spread of the virus delta through the liver, its tissues and cells begin to mutate or die, which not only complicates the work of the organ, but the whole organism. Diet for hepatitis D can reduce the load on the liver and accelerate its recovery during therapy. Changing the diet is a prerequisite for a full recovery and implies the rejection of a number of products:
- Spicy and fried foods.
- Fast food.
- Excessively salty or sweet foods.
- Alcohol.
 The diet should consist of dietary meat (poultry, rabbit), low-fat dairy products (cottage cheese, kefir), healthy fats (avocados, olive oil) and carbohydrates (grains), as well as a large amount of fresh fruits and vegetables. During inpatient treatment, a dietary table No. 5 is prescribed.
The diet should consist of dietary meat (poultry, rabbit), low-fat dairy products (cottage cheese, kefir), healthy fats (avocados, olive oil) and carbohydrates (grains), as well as a large amount of fresh fruits and vegetables. During inpatient treatment, a dietary table No. 5 is prescribed.
Mandatory in therapy is the abandonment of alcoholic beverages, smoking and taking narcotic substances.
Complications and consequences
Inflammatory processes in the liver caused by the hepatitis D virus, with proper treatment, can be completely stopped. The acute form of the disease either leads to recovery, or takes on a chronic form, which is much worse for therapy. A fatal outcome in acute hepatitis is possible in 1% of all patients, in the case of the development of the fulminant form, this is a severe stage of the disease, manifested by necrosis of the cells and hepatic coma. About 80% of these patients die.The least dangerous consequence of the acute form of the virus delta is dyskinesia of the biliary tract, when the production and withdrawal of bile is disturbed in the body, and, as a result, problems with the gastrointestinal tract.
Chronic hepatitis D is the most dangerous, since its result is cirrhosis of the liver (20% of cases) or malignant formations in it. Depending on the strength of the immune system, cirrhosis and cancer can develop within 20 years after infection with the virus.
Life forecast
Modern medicine gives very positive predictions for hepatitis B and D. The acute form of pathology is almost always treatable and only in 10% of cases leads to a chronic stage. Patients after the acute form can live long and fully.
 However, the presence of superinfection in the body, which was the result of the development of an infection of genotype D against the background of chronic genotype B, in 90% of cases goes into a chronic form and leads to complete liver damage. Life expectancy with a similar form of genotype D infection is from 2 to 20-30 years, depending on the strength of the body and immunity.
However, the presence of superinfection in the body, which was the result of the development of an infection of genotype D against the background of chronic genotype B, in 90% of cases goes into a chronic form and leads to complete liver damage. Life expectancy with a similar form of genotype D infection is from 2 to 20-30 years, depending on the strength of the body and immunity.
Virus prevention
The most effective way to prevent hepatitis D - vaccination against hepatitis B. Today it is the simplest and most affordable option for preventive measures.
For protection, it is also worth avoiding dubious beauty salons and tattoos that do not have quality certificates, as well as being protected during sexual intercourse with an unverified partner. You should regularly undergo an examination with an infectious disease specialist and take all the necessary tests every six months for the timely detection of the disease.
 Hepatitis D is not a fatal and incurable disease, you only need to take care of your health in advance - get vaccinated and be observed by a doctor. Simple and uncomplicated actions can save lives and health.
Hepatitis D is not a fatal and incurable disease, you only need to take care of your health in advance - get vaccinated and be observed by a doctor. Simple and uncomplicated actions can save lives and health.












