Despite the huge technological potential of modern medicine, the use of blood transfusion is still an indispensable procedure.
A method involving a blood transfusion is considered risky. However, in certain situations, it can be used to save not only health, but also human life.
Material Content:
- 1 What is blood transfusion?
- 2 Types of Blood Transfusion
- 3 Biological compatibility test
- 4 Indications and preparation for the procedure
- 5 Transfusion technique
- 6 Transfusion media and preparations
- 7 Blood transfusion to a newborn baby
- 8 Possible complications of blood transfusion
- 9 Contraindications to the procedure
What is blood transfusion?
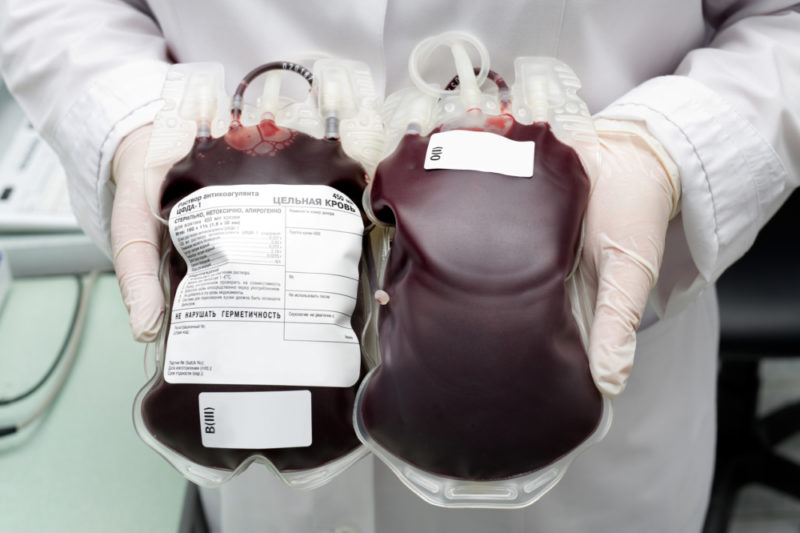
Blood transfusion is a medical procedure in which donor blood is transfused to a recipient - either directly or using canned material.
The first attempts at blood transfusion were made back in the 17th century, when the blood circulation of a person was discovered. Success in this direction came to physicians much later - after scientists learned to distinguish and determine blood groups.
The intake of physiological fluid for long-term storage is carried out at blood transfusion stations or in other specialized institutions.
The procedure for donating blood is voluntary. The resulting material is examined for infections, then stabilized and canned using special additives. In addition, donor blood serves as a source for obtaining blood particles - red blood cells, platelets and plasma.
Subsequently, the extracted components are used to replace the missing particles in the patient’s blood or on their basis produce drugs that restore and maintain the volume of circulating blood flow.
Finding a body fluid with perfect parameter compatibility is extremely difficult. Therefore, whole blood transfusion is rarely practiced - only in cases of urgent need for direct blood transfusion.
Types of Blood Transfusion
The blood transfusion procedure differs by the method of execution and the method of blood supply. The choice of this or that type of transfusion is determined by the specifics of the tasks set by doctors and the state of health of the patient.
The main methods of blood transfusion:
- intravenous - the basic, most common type of blood transfusion. Performed by inserting a catheter into the subclavian vein;
- intraarterial - used in exceptional cases, for example, with cardiac arrest;
- intraosseous - blood is injected into the iliac bone or into the skeletal part of the sternum;
- intracardiac - blood transfusion into the left ventricle is performed in cases where it is not possible to apply other methods of injecting biological fluid;
- intra-aortic - is used only in emergency situations.
Direct blood transfusion provides for infusion directly from the vein of the donor using specialized medical equipment that provides a continuous supply of biological fluid.
Indirect blood transfusion - a procedure in which conserved donor material is used.
In addition, there are alternative types of blood transfusion:
- exchange, in which part of the blood is previously pumped out from the recipient, and then donor material is introduced;
- autohemotransfusion - a method of using pre-preserved blood of the patient himself;
- reinfusion - reuse of blood poured and collected during surgery.
The rate of infusion of biological fluid depends on the type of infusion - drip, jet or jet-drop. The choice of procedure parameters is entirely within the competence of the doctor.
Biological compatibility test
The individual blood parameters for all people are different, even if they are close relatives. The exception is only identical twins.
Therefore, to avoid rejection, doctors check the infusion material for compatibility with the blood of the recipient.
As a rule, a biological compatibility test takes place in three stages:
- 15 ml of donor material is poured into the patient jet;
- within three minutes, indicators of the state of the recipient are monitored - pulse rate, respiratory rate, blood pressure, the occurrence of edema in the face;
- in the absence of adverse reactions, the procedure is repeated two more times.
If a triple check showed no complications, then the infused blood is compatible with the biological parameters of the patient.
In patients under general anesthesia, stability of hemodynamic parameters and general indicators of their condition are considered evidence of blood compatibility.
The presence of incompatibility is evidenced by such reactions as: difficulty breathing, decreased pressure, increased heart rate, chest pain, and often pain in the lumbar region.
Indications and preparation for the procedure
According to the degree of relevance, indications for blood transfusion are divided into absolute and relative. Absolute is the condition of the patient when a blood transfusion is regarded as the only way to stabilize him and avoid death.
The use of blood transfusion is especially important for acute blood loss, traumatic shock or extensive surgical interventions that caused the loss of a large amount of blood.
Relative indications include conditions when blood transfusion is regarded as an auxiliary, but not mandatory therapeutic measure.
In the list of main relative indications:
- anemia of any etiology;
- inflammatory processes accompanied by severe intoxication;
- bleeding disorders;
- vitamin deficiency, exhaustion due to starvation or chronic pathology;
- hemorrhagic diathesis.
Donor blood infusions can replace the volume of lost blood, restore gas exchange function, strengthen the immune potential and ensure the normalization of coagulation.
Features of the preparatory period
Preparation for a blood transfusion is designed to exclude the development of adverse reactions and complications, as well as reduce the sensitization of the body.
The most important point in preparing for the procedure is the determination of the blood group and the Rh factor of the patient and donor material, and the comparison of the data obtained.
Compatible is the blood of the same group affiliation and Rh factor.
In addition, the duties of the doctor include a complete collection of the patient’s medical history, namely the presence of:
- tendency to allergies;
- chronic diseases;
- contraindications for blood transfusion;
- previously transferred blood transfusions.
If the patient is a female patient, the doctor will determine if she had a birth and how they went. In some cases, an additional examination is prescribed to determine the antibodies.
In addition, a few days before the procedure, the patient is advised to limit the intake of protein foods. And immediately on the day of blood transfusion, care must be taken to ensure that both the intestines and the bladder are not full.
All these steps of the preparatory period are relevant only with the planned blood transfusion.
In the presence of absolute indications, the need for preparatory measures for the procedure is determined by the doctor.
Transfusion technique
Technical features of blood transfusion are directly dependent on the type and method of performing blood transfusion.
In direct transfusion, only whole biological material is used that does not contain stabilizers, which retains all cellular and protein elements, as well as coagulation characteristics.
Direct transfusion involves connecting the donor vein to the vein of the recipient through a special apparatus installed between the donor and the recipient.
After a venipuncture, a small amount of saline is administered to the patient. Then, a donor vein is punctured and a part of the apparatus tube is attached to the needle. Blood is injected in portions of 25 ml. The standard rate of hardware blood transfusion is 75 ml of blood per minute.
Specifics of performing indirect transfusion
For indirect transfusion, special equipment is used - a system equipped with short and long tubes (rubber or plastic), needles, filters and a dropper with a clamp. Such systems are classified as disposable and are available in sterile packaging.
One of the needles is inserted into a bottle with biological material, the second into the patient's vein. One of the rules implicitly followed by doctors is that canned blood is only transfused from the container in which it is packaged.
The rate of blood injection is regulated using the clamp, which is equipped with one of the rubber tubes. The standard transfusion rate is 50 drops per minute. Blood transfusion is completed if 20 ml of biological fluid is left in the vial. The needle is removed from the patient's vein, and a bandage with an antiseptic is applied on top.
The remaining 20 ml of blood is stored in the refrigerator. If a patient experiences complications, this material will be examined to determine the cause of the adverse reaction.
Transfusion media and preparations
To perform blood transfusion, whole blood is used, as well as its cellular and non-cellular components.
Donated blood for direct transfusion is considered the most effective transfusion medium. Its significant drawback is the rapid coagulability, which provokes the occurrence of thromboembolism.
Canned blood is prepared on the basis of whole blood with the addition of stabilizing and preserving components - sodium hydrocitrate, glucose, phosphate. The use of whole canned blood is appropriate for extensive blood loss.
The main disadvantage of biomaterial is a short shelf life and a gradual loss of functional properties within six hours after harvesting.
Cellular components are called particles extracted from a solid fluid. Based on them, such transfusion media are created as thromboconcentrate, erythrocyte mass or suspension, granulocytes, leukocyte mass.
Complex preparations include non-cellular components - plasma, albumin, serum, protein, immunoglobulins, prothrombin complex, cryoprecipitate, autohemophilic globulin, fibrinolysin.
Blood transfusion to a newborn baby
Blood transfusion for newborns is carried out in the presence of the same indications as in adults.
The most common indication for blood transfusion of newborns is hemolytic jaundice. For the treatment of pathology, the introduction of an erythrocyte mass, separated from platelets and leukocytes, is prescribed.
The choice of dosage is performed by the doctor individually, taking into account the characteristics of the body of the newborn.
Possible complications of blood transfusion
The blood transfusion procedure can cause the development of post-transfusion reactions or complications.
Reactive manifestations - nausea, fever, cyanosis of the lips, fever, are extremely rare and usually do not cause dysfunctions of internal organs.
While complications of blood transfusion pose a threat to the life of the patient, since they can cause serious disruptions to vital organs:
- air embolism - the penetration of air bubbles into a vein;
- thromboembolism - clogging of arteries with blood clots that formed during storage of biological fluid;
- blood transfusion shock - the result of blood incompatibility in a group or Rh factor;
- hemolysis - acute or delayed. Accompanied by the destruction of red blood cells;
- citrate or potassium intoxication - observed with an excess of stabilizing biomaterial substances;
- massive blood transfusion syndrome - occurs with excessive blood infusion for a short period of time;
- viral or bacterial infection.
The appearance of transfusion complications indicates a violation of the rules of the procedure or the use of biomaterials incompatible with the patient’s blood.
Contraindications to the procedure
The number of contraindications for a blood transfusion significantly exceeds the list of situations in which this procedure may be useful. Moreover, if you do not take into account or ignore contraindications for blood transfusion, the procedure can cause serious health problems.
It is strictly forbidden to conduct a blood transfusion for patients who are diagnosed with:
- acute organ failure - heart, liver, kidney;
- active tuberculosis;
- myocardial infarction;
- inflammation of the heart muscles;
- heart defects;
- thrombosis;
- pathology of cerebral circulation.
Blood transfusion is often the only chance to save a patient’s life. And the main task of doctors is to minimize the risk of complications and adverse reactions.