Hemorrhagic diathesis is a difficult to treat group of hereditary congenital and secondary hematological diseases, the basis of which is a disorder of a complex of organismic reactions aimed at preventing and stopping blood loss. These disorders pose a high threat to health and are a causal factor in the development of a large number of other pathologies. In total, more than three hundred varieties of this type of diathesis are registered in medical sources.
Material Content:
What is hemorrhagic diathesis
Hemorrhagic diathesis is a generalized name for a number of severe congenital or acquired blood diseases in case of impaired hemostasis (coagulation system), which are characterized by the development of spontaneous or heavy bleeding or hemorrhage, the degree of which does not correspond to the depth of the traumatic factor.
Classification
The disease is conditionally divided into 2 groups:
- The primary (congenital) form, which has a hereditary character and is caused by a gene mutation. Identified in early childhood.
- Acquired (symptomatic, secondary) pathology that provokes blood and vascular diseases. According to indicative medical data, approximately 5 million people in the world are diagnosed with a primary form of the disease, but in conjunction with secondary hemorrhages, the pathology is much wider.
In addition to this division, there is a widely used classification of hemorrhagic diathesis in medicine, formed in accordance with which specific hemostatic factor is impaired (vascular, plasma-coagulation, platelet).
Based on this classification, three basic types of disease are distinguished:
- Thrombocytopenia. Painful conditions against the background of an abnormal decrease in the number of platelets - blood elements that mature in the bone marrow and are responsible for blood coagulation in case of damage. This group also includes thrombocytopathies, which are characterized by insufficient activity of the platelets themselves. Both pathologies are characterized by abnormal bleeding. These conditions include such forms of the disease as essential thrombocythemia, idiopathic thrombocytopenic purpura, impaired platelet function in leukemia, hemorrhagic aleukia.
- Coagulopathy Hemorrhagic conditions due to a weakening of the functions of anticoagulant factors and a violation of the phases of blood coagulation. Among them are hemophilia, hemorrhagic diathesis of newborns, hypoproacetalinemia (parahemophilia), a reduced amount of prothrombin (factor P) after an overdose of drugs that thin the blood, DIC, hypoproconvertinemia, afibrinogenemic purpura, von Willebrand disease and Stuart Prouer.
- Vasopathies that occur against the background of various lesions of the walls of the vessels: hemorrhagic vasculitis, angiomatosis, purpura.
Causes of the disease
The key causes of painful conditions are defects in the function of hemostasis, which normally support normal blood flow, stop bleeding and dissolve blood clots.
With quantitative or qualitative deviations from the norm, coagulation factors develop hemorrhagic pathologies.
Primary (hereditary) types of the disease (Glanzmann thrombosis, hemophilia, Randu-Osler and Stuart Prouer diseases) are determined by congenital insufficiency of most often one factor.
The emergence of secondary (acquired) forms cause defects in several factors of hemostasis, which in turn provoke diseases such as:
- hemorrhagic fever of any type, including Ebola;
- immunodeficiency states;
- autoimmune diseases, including systemic lupus erythematosus;
- viral infections;
- bacterial endocarditis;
- cirrhosis of the liver, renal pathology;
- acute vitamin deficiency C, K.
Symptoms and signs
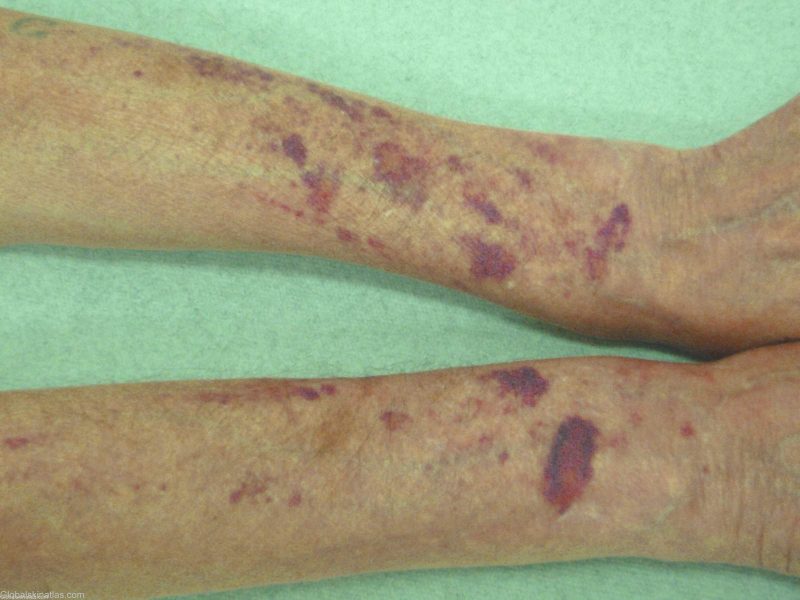
Common underlying symptoms for any type of hemorrhagic diathesis:
- syndrome of increased bleeding (hemorrhage), which is expressed in repeated, long-term non-stop bleeding of varying intensity and hemorrhages in different parts of the body and in the tissues of organs;
- posthemorrhagic anemia.
Bleeding with different types of disease is manifested by specific symptoms. Their intensity is determined by the cause, type of disease, concomitant complications, and varies from small subcutaneous hemorrhages to deep tissue hematomas and severe bleeding.
| Type of bleeding | Type of disease | Specific symptoms |
|---|---|---|
| Microcirculatory (capillary) | Thrombocytopathy, thrombocytopenia | • petechiae (pinpoint hemorrhages) on the skin and mucous membranes, including the oral cavity, nose, genitals, eye proteins, bruises, red and violet spots arising from slight damage to small vessels (squeezing hands, rubbing the skin, measuring pressure, slight bruising); • bleeding from the gums, uterus, nose, from the hole after tooth extraction. |
| Hematoma | Hemophilia, an overabundance of anticoagulant drugs | • painful dense subcutaneous hematomas, an outpouring of blood into the articular cavities (hemarthrosis), fatty tissue, retroperitoneal tissues; • abnormal fractures with mild bruises, destruction of bone and cartilage (deforming osteoarthrosis), contractures - limitation of mobility during abnormal contraction of tendons, skin, joints caused by large hematomas. |
| Capillary hematoma (mixed) | Von Willebrand disease, overdose of blood thinners, DIC | The combination of manifestations of capillary and hematoma type hemorrhages |
| Microangiomatous | Angiomatosis, abnormal fragility of capillaries against the background of increased permeability of their walls | • recurrent nosebleeds, sometimes diagnosed in the stomach, lungs, intestines; • the presence of blood in urine, feces. |
| Vasculitis Magenta | Vasculitis | • symmetrically located point hemorrhages, which often occur on the body and leave residual pigmented spots; • joint pain with marked swelling; • nausea, spastic pains in the stomach, intestines, vomiting mixed with blood inclusions; • kidney damage (lumbar pain, protein in the urine, urinary retention). |
Frequent subcutaneous and tissue hemorrhages cause iron deficiency anemia, which is characterized by:
- increased weakness, sweating;
- pallor of the skin and mucous membranes;
- low blood pressure, chilliness;
- dizziness, fainting;
- heart palpitations.
Hemorrhagic diathesis in children also proceeds with symptoms characteristic of a particular type of pathology. Kids may complain of bruising, joint pain due to the formation of dense bruises in them, and abdominal discomfort (if there is stomach or intestinal bleeding). With damage to the renal vessels in the child, the color of urine changes, with the development of anemia, noticeable fatigue, pallor of the face are noted. Brain hemorrhages are also dangerous, leading to neurological disorders, overexcitation, convulsive phenomena, and mental retardation.
In younger girls, the development of diathesis of this type is often accompanied by profuse menstrual blood loss.
Differential diagnosis
An examination plan for making a diagnosis, determining the type of diathesis and the probable causes of its development is developed by a hematologist together with narrow specialists depending on the type of pathological manifestations. This may be a rheumatologist, a vascular surgeon, a gynecologist, an infectious disease specialist, or a traumatologist.
For the initial diagnosis of pathology carry out:
- standard and biochemical blood tests;
- urinalysis, feces for blood;
- detailed coagulogram - a broad analysis of a number of indicators of blood coagulation, designed to identify which factor in the hemostatic system is impaired.
Based on the results, extended studies are prescribed in order to establish the cause of hemorrhagic manifestations and develop treatment tactics.
The main among the diagnostic procedures:
- radiography of the chest, joints, electrocardiogram;
- Ultrasound of the abdominal region, ultrasound of the kidneys and liver;
- sternal puncture;
- Coombs test (for pathology caused by immune disorders);
- analysis for antiplatelet antibodies;
- determination of lupus anticoagulant;
- functional tests for fragility of capillaries;
- trepanobiopsy.
In addition to them, the patient undergoes other studies recommended by narrow specialists, including examination by a geneticist.
Differential diagnosis is necessary to accurately determine the type of hemorrhagic diathesis, since its different forms with similar symptoms require the use of specific medications in each case.
There are special differential diagnostic tests based on a set of specific symptoms characteristic of a particular form of the disease, such as bleeding, deficiency of coagulation factors, duration of bleeding, and level of fragility of capillaries.
Treatment of hemorrhagic diathesis
Treatment tactics are developed taking into account the identified underlying cause of the disease, the type of hemorrhagic diathesis, the severity of pathological manifestations of bleeding.
If life-threatening conditions develop, for example, extensive bleeding, cerebral hemorrhage, DIC, the patient is urgently sent to the hospital for intensive hemostatic therapy - measures to stop bleeding and restore lost blood volumes.
In other cases, patients are treated in a special hospital or at home, also using drugs aimed at preventing and quickly stopping hemorrhages.
Basic medications:
- With autoimmune thrombocytopenia, hormonal medications, immunosuppressive cytostatics, plasmapheresis are required.
- With thrombocytopathy, different hemostatic medicines are used (Tranexam, aminocaproic acid, Ethamsylate (Dicinon), Epsilon).
- Patients with a hereditary deficiency of a specific coagulation factor are given replacement therapy with their substitute concentrates (immune, hemophile M, Coate-Dvi, immunin, aimafix D, octanine). With hemophilia, blood and plasma injections, red blood cells, and modern anti-inhibitory complexes (Feib Tim 4 immuno) are performed.
- With vasculitis, platelet purpura, antiplatelet agents are prescribed - agents that prevent the formation of blood clots, anticoagulants to improve the flowing properties of blood and blood flow, glucocorticosteroids to suppress inflammatory phenomena in the perivascular tissues. Often prescribed antispasmodic medications, nootropics that improve brain function, funds that strengthen the vascular wall.
- In case of Randu-Osler disease (hemorrhagic angiomatosis), medications are prescribed to stop bleeding, cryotherapy, drugs that strengthen the walls of blood vessels - vitamins K, P and C, Rutin, Vikasol.
- With hemorrhages against the background of gastrointestinal pathologies, Dicinon, direct anticoagulants, NaCl infusions, antispasmodic drugs are used.
- With the development of DIC, which often develops with secondary hemorrhagic diathesis and leads to massive hemorrhage, emergency measures are taken to stop blood coagulation inside the vessels, transfuse blood, inject heparin, stop the shock using hormones, opiates, and dopamine.
If, due to frequent bleeding, the patient loses a lot of blood, the question of removing the spleen (splenectomy) is resolved.
Be sure to identify and treat the root cause of the disease - the one that led to the acquired hemorrhagic diathesis - allergies, digestive, liver pathologies, oncological processes in the spleen. After eliminating the disease provocateur, hemorrhages often subside.
Complications and prognosis
Common complications that accompany the disease are:
- anemia, which is eliminated by taking drugs with iron of the last generations and observing a special diet;
- partial paralysis caused by massive hematomas that compress the vascular and nerve plexuses - to eliminate large formations drain, removing clotted blood;
- joint contractures and stiffness of joints due to recurrent hemorrhages in the articular cavities (hemarthrosis) - the treatment consists in setting therapeutic drainage and pumping blood from the cavities;
- severe bleeding in the tissues and cavities of organs, cerebral hemorrhages (strokes), which pose a threat to life;
- infection with hepatitis virus, HIV during blood transfusions.
The intensity of hemorrhagic diathesis is determined by the form of the disease, age, severity of clinical symptoms. The prognosis largely depends on the severity of the manifested complications.
With a timely diagnosis, conducting competent and active therapy, the outcome of the disease is relatively favorable.If the pathology becomes malignant with frequent heavy bleeding and complications, the prognosis can be depressing.
Preventive measures
Prevention measures include:
- At the stage of planning conception, a genetic couple is examined by a geneticist, especially if one of the partners has relatives with congenital blood clotting disorders.
- Establishment of the fetal sex of an already pregnant patient and identification of mutant genes in him. Sometimes it is better to postpone conception and, through scientifically proven methods, increase the likelihood of having a baby of the same sex for which hemorrhagic pathologies are less likely. So, in a man with hemophilia, sons can be completely healthy. A woman with mutant genes (carriers of the disease) is desirable to have daughters.
- Periodic examinations of children and adults to diagnose hemorrhagic diathesis as soon as possible.
- Active treatment of concomitant vascular pathologies, internal diseases.
- Measures aimed at strengthening the immune forces (vitamin complexes, hardening, physical activity, a complete diet).
- Attentive attitude to the taken medicines, refusal of uncontrolled use.
- Immediate call to a specialist if there are disturbing signs.
- When planning surgical interventions - consultation and examination by a hematologist.
- Use in blood transfusions is not of the usual donor plasma, but exclusively of coagulation factors that are necessary for the testimony, which reduces the risk of aggravating the course of the pathology.
The study of the methods and means for providing emergency home care to the patient during bleeding is also essential.